Introduction
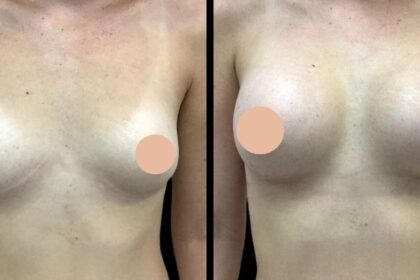
In the realm of regenerative medicine, platelet-rich plasma (PRP) has emerged as a cornerstone of biologic therapy, offering patients a treatment option that taps into the body’s natural healing potential. Among the various technologies available to clinicians, Tropocells PRP stands out as an efficient, easy-to-use, and scientifically robust platform. Designed to provide a high-yield, high-purity concentrate of growth factors, Tropocells is redefining clinical expectations across orthopedic, chronic pain and wound care practices.
But what exactly makes this device system different? And how can practitioners ensure they’re using it to its fullest potential? This guest post explores the key features, workflow, applications, and considerations for optimizing results with this advanced platform.
What Sets Tropocells PRP Apart?
Tropocells PRP is an FDA-cleared, CE-certified platform that enables clinicians to produce high-quality PRP with minimal blood draw and minimal variability between sessions. Its closed, sterile system integrates separation technology with standardized tubes and dual-spin protocols—features that reduce the dependency on operator skill and increase the reliability of biologic output.
The proprietary gel separation matrix within the system facilitates the precise layering of plasma components during centrifugation. As a result, platelets are concentrated without the unwanted presence of red blood cells or excessive white blood cells, making the end product ideal for use in tissues where inflammation needs to be avoided.
From a clinical standpoint, this matters. Outcomes with PRP are not just about volume; they’re about purity, potency, and predictability—three areas where Tropocells delivers measurable advantages.
PRP Collection and Workflow Efficiency
An essential element of any regenerative protocol is the collection and preparation phase. In a typical PRP procedure using Tropocells, the workflow consists of:
- Blood Draw
The process begins with the withdrawal of 10–20 mL of peripheral blood from the patient into pre-packaged collection tubes that already contain anticoagulant. - Initial Centrifugation
The first spin separates the red blood cells and buffy coat from the plasma. The internal gel barrier effectively isolates these layers, reducing the likelihood of contamination or manual mixing errors. - Plasma Collection
The platelet-containing plasma layer is carefully extracted using provided transfer tools. Because of the standardized separation achieved by the gel, this step can be done consistently without the need for precision pipetting. - Optional Second Spin
For higher platelet concentration, a secondary spin can be performed to further separate platelet-rich plasma from platelet-poor plasma. - Clinical Use
Once processed, the PRP is ready for immediate injection or topical application, depending on the indication.
This streamlined process allows clinicians to complete the PRP procedure in under 20 minutes, maximizing efficiency without compromising biologic quality.
Understanding the Role of a Reliable Platelet Rich Plasma System
Every biologic application begins with a device. The Platelet Rich Plasma system you choose plays a foundational role in the outcome of your regenerative therapy. Devices that are prone to user error or biologic contamination can compromise clinical outcomes and erode patient trust.
Tropocells minimizes these risks by offering:
- Standardized tube sizes and built-in anticoagulant handling
- A proprietary separation gel that reduces platelet loss
- Dual-spin options for practitioners seeking customized concentrations
- Single-use components for better sterility control
Unlike improvised methods or less refined systems, Tropocells delivers both concentration and consistency. And in regenerative care, consistency translates directly to clinical confidence.
Versatile Applications Across Specialties
The versatility of Tropocells PRP extends its relevance across a wide array of specialties. In orthopedic and sports medicine, it’s commonly used to manage tendon injuries, mild osteoarthritis, and muscle tears.
PRP is used to enhance bone grafting, reduce post-surgical healing time, and improve soft tissue recovery. Wound care centers, particularly those handling chronic ulcers, value Tropocells for its ability to deliver autologous growth factors to poorly vascularized tissue.
This multi-specialty adaptability makes it not only a practical tool, but also a cost-effective investment for clinics offering diverse services.
Best Practices for Optimizing Outcomes
To ensure success with Tropocells PRP, it’s essential to focus on more than just the centrifuge. Consider the following best practices:
- Patient hydration: A well-hydrated patient yields better plasma volume during blood draw
- Anticoagulant integration: Ensure gentle inversion of collection tubes to avoid clotting
- Minimize processing delay: Use PRP within 30–45 minutes of preparation to preserve biologic activity
- Gentle handling: Avoid shaking or over-handling plasma to reduce risk of premature activation
- Clinical timing: Consider the stage of healing; PRP may be more effective in subacute than in chronic conditions
Clinical judgment paired with a predictable system can maximize patient satisfaction and procedural success.
Scientific Backing and Quality Control
Behind the performance of Tropocells PRP lies a foundation of peer-reviewed validation and quality manufacturing standards. Independent studies have shown that the system yields high concentrations of platelets while minimizing red cell contamination—important when delivering growth factors to sensitive or inflamed tissues.
Moreover, the manufacturer’s ISO 13485 certification ensures that the device is made in accordance with rigorous medical device quality management systems. These credentials add to the growing body of evidence that supports its adoption in both private practices and hospital settings.
Patient Communication and Post-Treatment Care
One of the often-overlooked aspects of PRP-based therapy is patient education. Clinicians should inform patients about what PRP is, what to expect during and after the session, and how outcomes may vary depending on individual biology.
After Tropocells PRP injections, mild soreness or swelling is normal, especially in joint or tendon applications. Patients should be advised to rest the treated area for 24–48 hours and avoid anti-inflammatory medications unless directed. Follow-up appointments may be necessary for evaluation or additional treatments.
Conclusion
In a field where biologic consistency, ease of use, and patient outcomes matter, Tropocells PRP offers a solution that’s engineered for modern clinical demands. Its closed system, dual-spin flexibility, and proprietary separation matrix make it a reliable choice for practitioners who want to elevate their regenerative therapy protocols without adding complexity.
By combining convenience with precision, this Platelet Rich Plasma system supports clinicians in delivering high-value care—whether the goal is pain relief, tissue regeneration, or functional recovery.